If you’ve ever felt a clicking, aching, or locking sensation in your jaw, you’re not alone. Jaw pain is something many people simply put up with—often thinking it’s “just stress” or something they’ll have to live with. But your jaw plays a vital role in daily life, and pain in this area can affect everything from eating and speaking to sleeping well. The good news? TMJ pain is very treatable, and Osteopathy can play an important role in reducing discomfort, improving mobility, and supporting long-term recovery.
For personalised advice or to see an osteo in Rosanna, contact our team at Excel Body & Health today.
Understanding the TMJ
Dysfunction in this joint is known as temporomandibular dysfunction (TMD). It’s more common than many realise, affecting an estimated 60–70% of the population at some point. It occurs most frequently in adults aged 20–40 years, and women are up to four times more likely to experience it.
Common Signs and symptoms of TMD
TMD can range from mild discomfort to severe pain that disrupts daily activities.
Typical symptoms include:
- Jaw pain or tenderness (especially in front of the ear).
- Clicking, popping, or grinding noises with jaw movement.
- Limited or uneven mouth opening.
- Jaw locking in an open or closed position.
- Headaches (often around the temples or behind the eyes).
- Ear pain, ringing (tinnitus), or a sensation of fullness.
- Facial muscle fatigue or tightness.
- Neck and upper back tension.
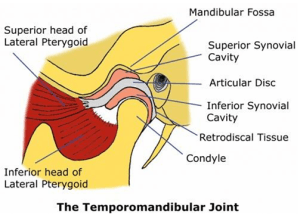
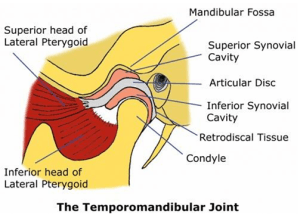
How the TMJ Works — and Why It Hurts
The TMJ is a complex joint with both hinge and gliding movements. Its key components include:
- Mandibular condyle: the rounded “ball” of the jawbone.
- Articular fossa: the “socket” in the temporal bone.
- Articular disc: a cushion between the two bones that helps the joint glide smoothly.
- Ligaments and capsule: providing structure and stability.
- Muscles of mastication: such as the masseter, temporalis, and pterygoids, which generate movement and control.
When everything works well, this system moves fluidly and pain-free. But if the disc becomes displaced, the muscles tighten, or the joint becomes irritated, the result can be pain, clicking, stiffness, or locking.
Common Causes and Contributing Factors
TMD can be triggered by one factor or a combination of several. Common contributors include:
- Teeth grinding or clenching (bruxism) – often during sleep or periods of stress.
- Emotional stress – leading to jaw tension and increased muscle activity.
- Poor posture – forward head posture places excess load on the jaw and neck.
- Overuse – chewing gum, biting nails, or pen chewing.
- Dental issues – misalignment, missing teeth, or recent dental work.
- Joint hypermobility – excessive movement that can lead to disc displacement.
- Trauma – such as a blow to the face or whiplash injury.
- Underlying medical conditions – like fibromyalgia or rheumatoid arthritis, which can make the joint more vulnerable.
What to Expect at an Osteopathy Appointment
When you see an Osteopath for TMJ pain, your session starts with a comprehensive case history. This helps us understand:
- How long you’ve experienced pain.
- Triggers or habits that may be worsening symptoms.
- Relevant dental or injury history.
- Associated symptoms such as headaches or neck stiffness.
Examination may include:
- Postural assessment — focusing on the cervical spine, upper back, and head position.
- Jaw movement tests — observing range, quality, and tracking of movement.
- Palpation — feeling for tension in the jaw and surrounding muscles.
- Functional assessment — checking how the disc and joint behave during opening and closing.
This thorough assessment guides a treatment plan tailored specifically to your needs.
Osteopathic Treatment Techniques
Osteopathy focuses on restoring function, improving mobility, and reducing pain.
Common treatment techniques may include:
- Soft tissue massage — easing muscle tension in the jaw, neck, and shoulders.
- Myofascial release — freeing tight fascia to improve fluid movement.
- Muscle Energy Techniques (MET) — gentle contractions to restore joint balance.
- Trigger point therapy or dry needling — releasing tight, overactive muscles.
- Joint mobilisation and articulation — restoring proper movement of the TMJ and surrounding joints.
- HVLA techniques — where appropriate, to address restrictions in the cervical or thoracic spine.
Because the TMJ works in harmony with the rest of the body, treatment often extends beyond the jaw — addressing the neck, upper back, and posture.
Self-Management Strategies
Long-term relief comes not only from hands-on treatment but also from empowering patients with self-care strategies. Your Osteopath may recommend:
- Jaw relaxation techniques — resting the tongue gently on the roof of the mouth, teeth slightly apart, lips closed.
- Heat therapy — warm compresses to ease muscle tightness.
- Gentle mobility exercises — improving control and coordination.
- Stress management — breathing, mindfulness, or relaxation techniques to reduce clenching.
- Posture correction — adjusting ergonomics at work and avoiding prolonged slouched positions.
- Avoiding aggravating habits — such as gum chewing, nail biting, or jaw tensing during concentration.
These strategies can significantly reduce pain flare-ups and support long-term recovery.
Why Addressing TMJ Pain Matters
Untreated TMJ pain can impact more than just your jaw. Many people experience:
- Ongoing pain radiating to the face, temples, or neck.
- Headaches and ear discomfort.
- Trouble eating, speaking, or concentrating
- Sleep disturbances
- Increased stress and lower quality of life
Early, targeted management can make a huge difference in preventing chronic pain and maintaining overall well-being.
How We Can Help
At Excel Body and Health, we provide personalised, evidence-informed care to help you understand and manage your TMJ pain. Through a combination of gentle hands-on treatment and practical self-care strategies, we aim to reduce pain, improve movement, and support lasting results.